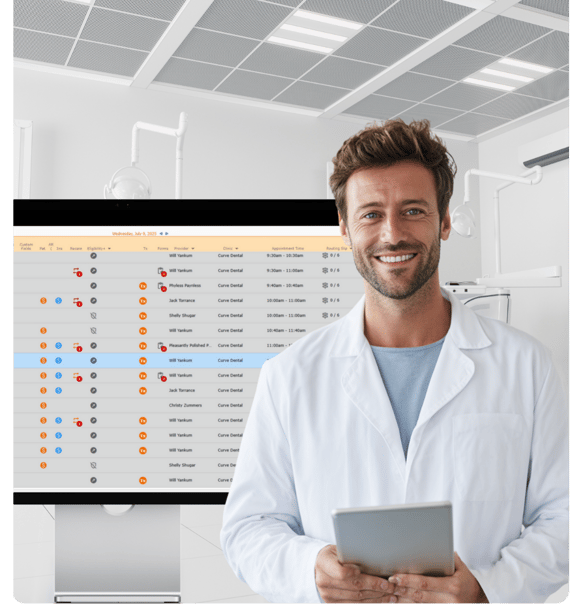
AI-Powered Dental Insurance Verification
Automate eligibility checks, reduce manual work, and get in-depth dental coverage details—fast. Fully integrated with Curve, so it works right inside your existing workflow.
Your Team Can Do More—
When They’re Not Stuck on Hold.
Eligibility+ is a fully automated, AI-powered dental insurance verification solution—built right into Curve. It checks patient benefits for you, pulling real-time, code-level coverage straight from payer portals.
No more juggling calls or logging into multiple sites. Just comprehensive eligibility details before the patient arrives, so your day runs smoother, your team saves hours, and patients know exactly what’s covered.
.png)
What makes Eligibility+ different?
Most verification tools hand you a pile of raw insurance data and make you dig for the differences.
SmartSync technology within Eligibility+ takes that work off your hands. It pulls accurate, code-level data from payer portals, automatically compares it to what’s in Curve, and flags anything that doesn't match.
All you do is review, approve, and watch SmartSync instantly populate the updates in Curve — turning hours of busywork into a few quick clicks.
That means no surprises, fewer errors, and a workflow that puts you in control.
Insurance Verified.
Work Simplified.
AI-Enabled Insurance Verification
Reduce the manual work with Eligibility+. Available with a Curve subscription.
15–30 min
Saved per patient
40%
Reduction in admin workload
20%
Boost in treatment acceptance
150%
Increase in same-day acceptance
Listen to What the Experts are Saying

Dr. Scott Leune: Eligibility+ Testimonial

Cassie Tallon: Eligibility+ Testimonial

Dr. Eric Roman: Eligibility+ Testimonial
.png?width=2565&height=2565&name=Testimonial%20Image%20(1).png)
"Eligibility+ has cut down the time we spend on insurance by hours every week! Now my team isn’t stuck on the phone or jumping between portals. We can finally stay ahead."
Dr. Williams
DDS
How It Works: Manual vs. Eligibility+
Ever wonder how different your day could look with automated insurance verification?
The Manual Way
- Spend hours on hold with insurance or jumping between portals
- Type in patient benefits by hand (easy to miss or mistype details)
- Only get basic info, like “active” or “inactive” coverage
- Patients wait longer for answers and often delay treatment
With Eligibility+
- Checks insurance automatically—no calls, no logins
- Pulls real-time, code-level coverage straight from payer portals
- SmartSync shows any differences between your system and the payer portal, and updates your records for you (with your approval)
- You have granular benefits information before the patient arrives, making it easier for patients to accept same-day treatment
Patients Feel Informed—and Say “Yes” With Confidence
Clear coverage upfront builds trust at check-in and makes it easier for patients to move forward the same day.

Upfront Clarity
Thorough eligibility data before the visit—no surprises at checkout.
Faster Check-In
Less back-and-forth, more time face-to-face with your team.
Easier “Yes”
Clear numbers make it easier to say “yes” to same-day treatment.
Ready for Insurance Verification Without the Guesswork?
When you take manual insurance checks off their plate, you give your team the freedom to focus on what actually moves your practice forward.
