Simplify Dental Insurance Billing, Accelerate Payments
.png?width=170&height=170&name=Testimonial%20Image%20(1).png)
“I haven't found a single system that allows me to create the kind of synergy necessary for clean claims. Curve SuperHero is a custom suite that synergizes all of the key points to allow me to get the result of a clean claim. No more ping pong, all hole in one!”
Cassie Tallon
Founder & CEO of The Fractional Match

Automate Insurance Verification
Eligibility+ is Curve's AI-powered, dental insurance verification solution that dramatically reduces your team's workload and helps your patients say "yes" with confidence.
No portals. No paperwork. Just clarity—built right into Curve.
- Real-Time Eligibility Checks: Automatically pull code-level coverage directly from payer portals to free up your team’s time.
- Integrated Patient Coverage Insights: Show accurate out-of-pocket costs before treatment—boosting treatment acceptance and helping you collect more upfront.
- SmartSync Technology: Detects discrepancies between payer data and what's in Curve, so you can catch changes instantly and update records with total control.
Speed Up Your Claims Process
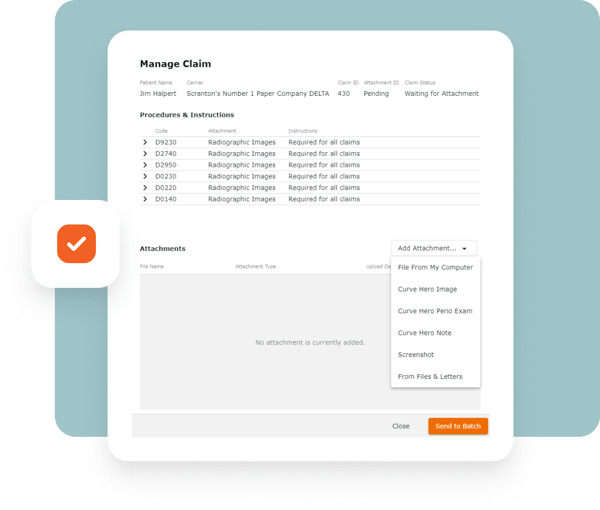
- Integrated Claim Attachments:
Attach and submit all required claim documents directly within Curve, eliminating the need to switch platforms and reducing errors for faster reimbursements - Smart Pop-Up Alerts:
Get automatic notifications when attachments are required for claims, reducing the risk of missing key documents and speeding up the reimbursement process
Watch this short video to learn how Cassie Tallon, a leading dental industry consultant on operational efficiency, unlocked the key to clean claims with Curve.
4 Ways Curve Accelerates Claim Reimbursement
Bill accurately in one click
Start clean with better intake
Follow Curve's best practices to reduce errors and avoid back-and-forth with insurance companies.
Connect charting to billing
Reduce write-offs, increase revenue
Catch mistakes early to protect your profits and collect what you've earned.
Clearer Insights, Faster Reimbursement
- Quick eClaim Submission and Tracking:
Submit and track claims at every stage, from clearinghouse to insurance processing to posting the remittance, all with just a few clicks - Electronic Remittance Advice (ERA):
Automatically receive and interpret ERAs, providing clear insight into claim status and reimbursement amounts
Boost Cash Flow with Instant, Error-Free Payment Posting
- Seamless Auto-Posting:
With Curve’s integrated payment solutions powered by Global Payments, insurance payments auto-post directly to the invoice, matching them line by line with the Explanation of Benefits (EOB).
What Auto-Posting Means for Your Practice:
- Auto-posting eliminates the need for manual entry, saving 5-7 minutes per patient and reducing errors.
- Faster, accurate posting leads to improved cash flow for your practice.
- Your team can focus on only handling exceptions, not routine payment tasks.
- With precise matches to EOBs, there’s less need for follow-ups with insurance companies.
- Auto-posting ensures payments are accurate, minimizing billing mistakes.
- You get clear, itemized payment insights, making reconciliation easier.
Frequently Asked Questions
Dental insurance billing is the process of submitting claims to dental insurance companies and tracking reimbursement for services rendered. Curve automates this workflow to reduce manual tasks and speed up payments.
Curve offers Eligibility+, an AI-powered dental insurance verification tool that automates time-consuming checks by pulling real-time, code-level data directly from payer portals. It syncs coverage details into your Curve workflow—giving your team accurate information, fewer surprises, and more time to focus on patient care.
Yes, Eligibility+ lets you automate verification for patients with SmartSync discrepancy detection and full control over updates, saving your team hours each week.
It's best to verify before every new treatment plan or annually at minimum. Curve lets you do this manually or set a recurring schedule with automated dental eligibility verification.
Every Curve subscription includes unlimited basic insurance eligibility checks at no additional cost.
If you need more detailed verification, Eligibility+ is available as a paid add-on, with tiered pricing based on monthly usage. It delivers real-time, code-level data pulled directly from payer portals—helping you reduce denials, collect more up front, and save hours each week.
